Stay Informed
Benetas newsroom features a collection of media releases, news, articles, and insightful opinions, all centered around the dynamic and evolving landscape of aged care.
Media Enquiries
Phone: 0400 224 852
Email: media@benetas.com.au
Our latest news
- Filter by category:
- Opinion
- Media Releases
- News Stories
- Support at Home

Category: Opinion
It is essential for providers to share their experiences of running wellness and reablement programs, so all in the sector can learn from each other, writes Sandra Hills.

Category: Media Releases
Physio-focussed pilot improves balance and reduces chance of falls to help seniors stay at home
Benetas home care clients have experienced benefits following a Wellness and Reablement pilot, which included twice weekly physiotherapy sessions.

Category: Support at Home
Support at Home: Changes to Home Care Funding
Support at Home is replacing Home Care Packages. Discover what’s changing in funding, services, and contributions for older Australians.

Category: News Stories
Mother's Day celebrations across our care homes
Our residents from Gisborne Oaks, Colton Close and The Views Heidelberg had a fantastic time celebrating Mother's Day!

Category: News Stories
Retirement Living Bowls Challenge
Dalkeith Heights residents have taken home the second Benetas Retirement Living Bowls Challenge.

Category: Opinion
Navigating aged care changes won’t be easy, but we can’t lose sight of the bigger picture
For the past 16 years, I have proudly served as Benetas CEO, guiding processes that help residents, clients and employees through societal changes both relevant and irrelevant to the aged care sector.

Category: Media Releases
Budget response – Pay increases welcomed but crucial support needed to implement once-in-a-generation sector reform
Benetas has acknowledged the Government’s commitment to funding pay increases for nurses in the Federal Budget, while calling for more clarity to allow the sector to safely implement crucial reforms.

Category: Media Releases
Macedon Ranges Health, in partnership with VicHealth, will run a two-week exhibition to help educate the community on the dangers of vaping.

Category: News Stories
Making dreams come true for our customers
Recently, we had the privilege of fulfilling a special wish for our home care client, Ruth.

Category: Media Releases
Bridgewater Lake Retirement Estate residents are eagerly preparing for their highly anticipated Craft Market, which will be held in the village’s community centre later this month.

Category: Support at Home
Support at Home program: Things You Need to Know
The new Support at Home program is coming soon: What You Need to Know. This new system aims to improve in-home care by reducing wait times, increasing access to services and ensuring funding is based on individual needs.

Category: News Stories
Clarinda residents bond over Bingo
Meet Kath and Trish, two of our wonderful residents and inseparable friends at Clarinda on the Park care home.

Category: Media Releases
Benetas has this week opened the first stage of its St Laurence Court Community, helping seniors secure affordable housing in Bendigo.

Category: News Stories
St Paul's Terrace residents dive into woodworking
Residents at our St Paul’s Terrace care home enjoy diving into the art of woodworking.

Category: News Stories
Eaglehawk resident Nell celebrates 100th birthday
Nell McDougall recently celebrated her 100th birthday alongside friends, family and fellow residents at Benetas Eaglehawk residential aged care home in Bendigo.

Category: Media Releases
Benetas Eaglehawk Bendigo resident marks sensational century
Nell McDougall celebrated her 100th birthday alongside friends, family and fellow residents at Benetas Eaglehawk residential aged care home in Bendigo last week.

Category: News Stories
Colton Close residents participate in friendly competition
Our Colton Close residents love coming together regularly for some friendly competition playing board games.
Category: News Stories
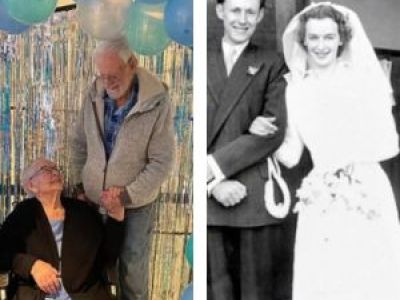
St Paul's Terrace residents celebrate 74th wedding anniversary
Our St Paul’s Terrace residents, Heather and John recently celebrated their 74th Wedding Anniversary surrounded by loved ones.

Category: Media Releases
Benetas welcomes Support at Home pricing announcement
Benetas has welcomed the Australian Government’s announcement that price caps on services under the Support at Home program will commence from 1 July, 2026.

Category: News Stories
Corowa Court residents knit for a good cause
Our Corowa Court residents love using their creative talents in support of a good cause.






